The Marshall Project highlights research on excess mortality in U.S. prisons:
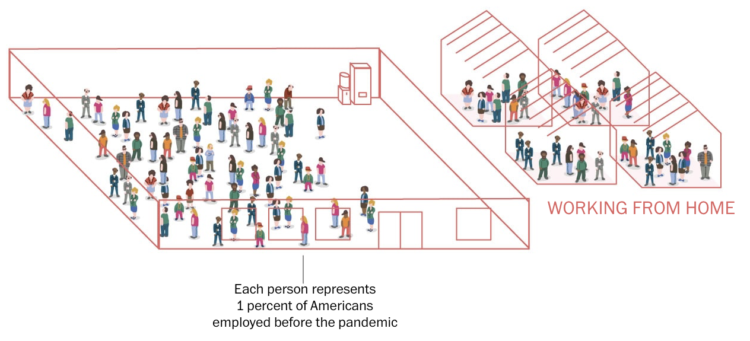
The slowdown in admissions meant that prison systems reduced the number of younger people exposed to COVID, while the older people already inside were left there. That’s because incarcerated people are generally older than those likely to be sent to prison.
By the end of 2020, Bureau of Justice Statistics data shows the number of people in state prisons under 55 fell by 17%, while the 55 and older population was down by 6%.
Prison deaths spiked almost everywhere across the country, varying in magnitude from state to state.
Tags: Marshall Project, mortality, pandemic