January is the time many of us make resolutions for the new year. Sometimes resolutions feel too big and long drawn out. As a result, our motivation to see them through can peter out before the end of the year.
Last year, we suggested 12 micro-resolutions to help you prepare your health for emergencies. Here are a dozen more ways to resolve to be ready this year.
January
Be prepared to prevent data loss. Data loss happens more often than you might think.
This month’s micro-resolution is to back up your important files. These include medical records, financial documents, family photos, and emails. Save at least one extra copy of your files to an external storage device or the cloud. This ensures you can still access the information if the original is lost, damaged, or destroyed.
February
February is National Canned Food Month. Canned goods are an emergency preparedness staple. And for good reason. They are reasonably affordable, require little to no preparation, and have a long shelf life.
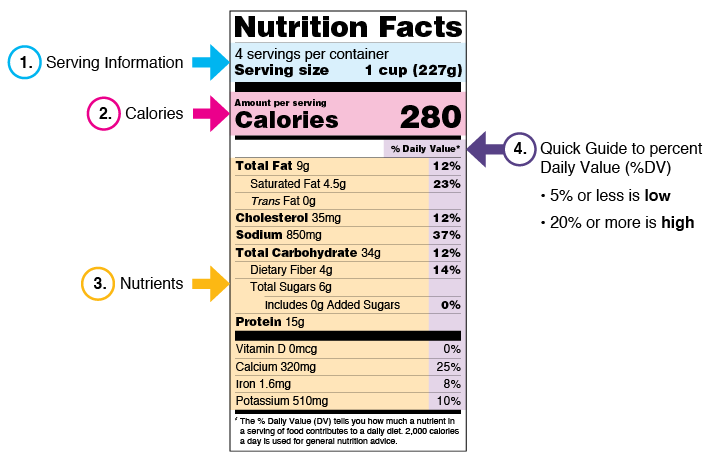
As often as people buy and cook with canned goods, some can find food labels confusing. This month’s micro-resolution is to improve your food label literacy. One way to do that is to get the FoodKeeper app to help you maximize the freshness and quality of the items in your emergency food supply.
March
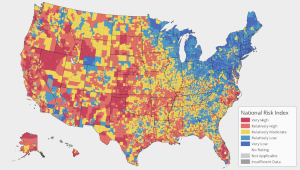
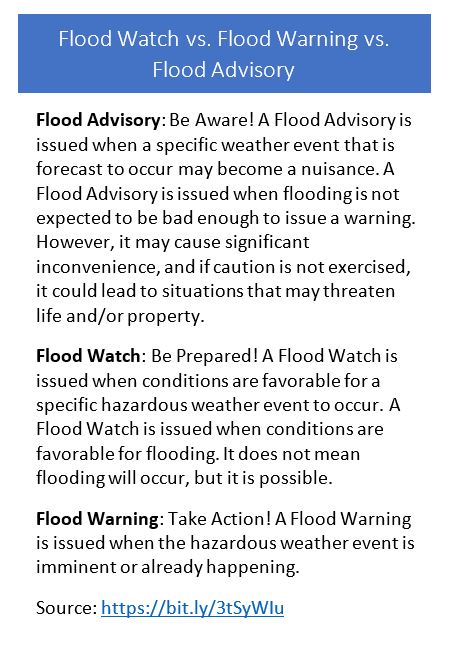
Severe weather, including tornadoes, can happen at any time of year. They are, however, more likely to happen in most places during the spring months(1)
This month’s micro-resolution is to take a SKYWARN® Storm Spotter Program class. You’ll learn:
- Basics of thunderstorm development
- Fundamentals of storm structure
- Identifying potential severe weather features
- Information to report
- How to report information
- Basic severe weather safety
Classes are free and open to the public.
Storm spotters are volunteers. They help keep their local communities safe by providing timely and accurate reports of severe weather to the National Weather Service.
April
April is National Financial Literacy Month.
Developing a habit of putting money aside—even if it is a small amount—is the easiest way to develop an emergency fund and build financial resiliency. Without savings, the financial shock of an emergency could affect you, your family, and your community.
This month’s micro-resolution is to download and fill out the “Your Disaster Checklist” (available in multiple languages). Use it to help you keep track of account numbers, valuables, medical information, and more.
May
May 5 is World Hand Hygiene Day. Effective handwashing is a practical skill that you can easily learn, teach to others, and use every day to help prevent the spread of illness and disease.
This month’s micro-resolution is for parents and caretakers. Teach the children in your care when and how to wash their hands.
June
June is Pet Preparedness Month. It’s also the start of the Atlantic hurricane season. What better time of year to practice evacuating with your pet:
- Train your pets to get in and stay in their carriers by making it a comfortable place.
- Take your pets for rides in a car like one you would evacuate in.
- Know where your pet might hide when stressed or scared. Practice catching your pet, if needed.
Have your entire family practice evacuating with your pets so everyone knows what to take, where to find the pets, and where to meet.
July
Most locations in the contiguous United States will experience their hottest day of the year between July 15-31.(2) Hot weather—regardless of when it happens and how long it lasts—can cause heat-related illness.
This month’s micro-resolution is to learn the symptoms of heat-related illness what to do if someone shows signs of heat stroke, exhaustion, or cramps.
August
August 20 is National Radio Day. Radio is one of many ways you can stay informed before, during, and after an emergency. Other ways include local television, social media, and Wireless Emergency Alerts (WEAs).
WEAs look like text messages. They are designed to get your attention with a unique sound and vibration repeated twice. This month’s micro-resolution is to check the settings on your mobile device to make sure you are receiving WEAs.
September
September is not just National Preparedness Month. It is also National Self-Care Awareness Month. Emergencies, including disease outbreaks and natural disasters, can cause increased stress. You and others might feel fear, anxiety, and other strong emotions. It’s important to take care of your family and friends, but it should be balanced with care for yourself.
This month’s micro-resolution is to find one small way each day to care for yourself. Yours might include:
- connecting with friends and family. Talking with people you trust about your feelings and concerns can relieve stress.
- showing kindness to others. According to researchers, helping others release hormones that boost your mood and wellbeing
- practicing relaxation techniques like meditation and deep breathing exercises. Relaxation techniques can help slow your breathing, lower blood pressure, and reduce muscle tension and stress.
October
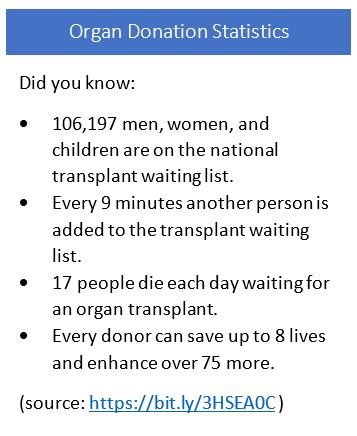
October is Health Literacy Month. People need information they can find, understand, and use to make the best decisions for their health every day. The same is true during an emergency when there’s usually an increase in the amount of information and speed at which it comes out.
One thing you can do to improve your health literacy is to ask questions of healthcare professionals. For example, your pharmacist is trained to help you manage and improve your health every day. They can give you patient-centered answers to questions on many topics, including emergency preparedness. Ask your pharmacist these questions the next time you visit the pharmacy.
November
Winter is coming. It may arrive in some parts of the country before the month end.
This month’s micro-resolution is to prepare your car for winter. Now is a good time to equip your vehicle with a roadside emergency kit. Winterize your ride with the following items:
- Food and water
- Ice scraper and a folding shovel
- A flashlight and batteries
- Car and portable chargers for your cellphone
- First-aid supplies
- Winter clothes, blankets, and sleeping bags
- Road flares
- Jumper cables
December
December is Hi Neighbor Month. Neighbors can be an important source of assistance in the hours, days, and weeks after an emergency. Because they live close—maybe even next door—neighbors might be your first and best option for help after a tornado or during a power outage.
This month’s micro-resolution is to find a way to get involved with your neighbors. Ways to get involved include
- offering to help your neighbors, especially people who are older, live alone or with a disability, or rely on electricity-dependent equipment, prepare for emergencies.
- involving trusted neighbors in your emergency action planning.
- joining an organization active in disaster, such as your local Medical Reserve Corps Unit or Community Emergency Response Team.
Resources
- Public Health Matters: Resolve to Be Ready
- Resolve to be Ready Social Media Toolkit (FEMA)
References
- https://www.nssl.noaa.gov/education/svrwx101/tornadoes/
- https://www.climate.gov/news-features/featured-images/if-things-go-%E2%80%9Cnormal%E2%80%9D-most-us-locations-will-have-their-hottest-day
Thanks in advance for your questions and comments on this Public Health Matters post. Please note that CDC does not give personal medical advice. If you are concerned you have a disease or condition, talk to your doctor.
Have a question for CDC? CDC-INFO (http://www.cdc.gov/cdc-info) offers live agents by phone and email to help you find the latest, reliable, and science-based health information on more than 750 health topics.