The worldwide spread of the SARS-CoV-2 virus, and the consequent Covid-19 disease pandemic, is still a topic of conversation, although it does seem that many people are sick of hearing about it. They just want to "get back to normal", without understanding that this is going to take many months, if it happens at all. There is every possibility that there will be a "new normal" from now on, and in many places the virus will be endemic.
We started off knowing little about this virus and the disease that it causes, as I have written about before (
There seems to be a lot of public misunderstanding about the coronavirus); and we have slowly accumulated more and more understanding of what we should be doing in response. In particular, the future of having to live with the virus is becoming clearer, until (or if) we reach herd immunity (
A new understanding of herd immunity).
Among all of this, there has been some commentary about the official response within Sweden, with some media (and the World Health Organization) claiming that the Swedes have reacted in a different and controversial manner. This is far from the truth, as I happen know, because I now live in Sweden, although I grew up in Australia. As a resident biological scientist, I thought that I might write about the situation, in this post. There have been massive quarantine efforts here, although for cultural reasons they might look quite different to how such things are organized in the English-speaking parts of the world. [Note: Japan has also used
a different strategy to most other places, but without any serious criticism, although it is now experiencing a serious "second wave".]
Many of the misleading media reports, have originated in the USA, which currently has the world's biggest Covid problem. The latter may soon change, because there is every reason to expect India to surpass the US infection count, as its rate is still rapidly increasing and India has a much larger population. I hope to be wrong on this matter, but it will be very hard to contain spread among the masses of poor people in that country. Maybe their saving grace will be the fact that the majority of their population is younger than 40 years old, so that the death rate will be contained.
Anyway, we have had US media reports about Sweden such as these:
The latter article contains this quote:
At one end of the spectrum, Sweden chose to forgo severe restrictions on public life and its economy and opt to let the virus spread through its population while shielding the most vulnerable groups.
Both pieces of information here are wrong. Sweden has
not allowed the virus to spread, but has instead instituted quarantine measures; and it
has failed miserably in its efforts to protect the prime vulnerable group: the elderly.
Virus spread in SwedenLet's start by looking at the actual data. Here is a table of the current officially reported number of SARS cases as of July 18 (as collated on the
Worldometer web site). Note that the information we are interested in is the case rate (percent of population affected), not the number of cases. The number of cases is determined mainly by the population size — of course the USA has more cases than Sweden, for example, because there are 330 million Americans and only 10 million Swedes.
As you can see, the case rate in the USA is 10,500 per million people, whereas in Sweden it is only three-quarters of this, at 7,500 cases. So, who is doing better at containing the spread of the virus? Mind you, within Europe, only Armenia and Luxembourg have higher reported rates, along with tiny places like San Marino, Andorra and the Vatican City (where even a few cases can create apparent large rates, due to the small sample size).
Moreover, the number of new cases per day in Sweden is now as low as at any time since mid March, as shown in this next graph (also from
Worldometer). The apparent burst in cases after June 5 was due to the government finally implementing large-scale virus testing, which always increases the detection rate for this type of situation. The subsequent decrease in cases suggests that Sweden may well be moving towards herd immunity, which is required for long-term epidemic control. This week's report from
Folkhälsomyndigheten (the Public Health Agency) shows a continue decrease in the proportion of positive tests, despite a continued high level of sampling.
The Swedish situation contrasts with the current
situation in the USA, where the number of new cases is higher than at any previous time, being double what it was during the April-June period. This is, at least in part, due to a massive sampling effort now on, which I noted above will increase the case detections.
The same trend can be seen in the number of new daily deaths in Sweden — it is now as low as at any time since mid March. The number of US deaths, on the other hand, has surged this month (although it is still less than a half of what it was back in April). Sweden may be a cautionary tale, perhaps; but the criticism sounds more like sour grapes, to me, from the media of a country that has clearly handled this pandemic worse than anyone else.
It is important to mention a point of difference, as it has become increasingly obvious that different jurisdictions have compiled coronavirus cases differently, even within the European Union.. As far as Sweden is concerned, there were apparently a lot of "active cases" early in the pandemic. However, what was happening was that most places were declaring cases as "recovered" after the person's symptoms receded, which takes about 7 days. On the other hand, Sweden did not officially declare a case recovered until the person was completely virus free, which takes about 5 weeks. So, Sweden's reported number of active cases remained much higher than most other places, for a much longer time, which may have generated a lot of the negative media publicity. This situation no longer applies, because the number of cases is much lower now.
I would hate to be the person who has to officially compile the worldwide data on this pandemic. Even the decision about what constitutes a "Covid death" differs between countries, with some jurisdictions including all people who test positive for the virus, irrespective of what they die of, and others counting only those cases where the virus is the main cause of death (eg. a cytokine storm). Trying to make the worldwide data comparable will not be easy.
Quarantine in SwedenSo, what has been different about Sweden? It is simply that the national government expects Swedes to take official advice when they are given it, without being forced to do so. In most cases, this actually works, although there will always be exceptions. In the case of this pandemic, the government simply gave everyone the same advice as everyone else in the world was forced to take. It really is as simple as that.
Where I spent the first two-thirds of my life, in Australia, such an approach would be laughable. because Australians do not respect their governments, state or national. So, without a police-enforced mandatory shut-down, the virus would have spread unchecked. You may have seen the media pictures of Sydney people jammed onto beaches when they were told not to go to work (
Famous Sydney beaches closed after crowds flout coronavirus restrictions); and you may have read about the complete failure in the Melbourne hotel used for quarantining international arrivals (
Breaches of hotel quarantine 'let Victorians down', Minister says as inquiry launched). There is nothing unexpected about this, even if I say this as an Australian citizen.
In contrast, Sweden's island summer-holiday destinations have had among the lowest infection rates in the whole country — Öland 0.3%, Gotland 0.3%, compared to a national total of 0.8%. I am not claiming that Swedes are more sensible than anyone else (or less!), merely that they take official advice without being forced. This may seem odd to you, perhaps, but it is true, as I can attest from living here for the past one-third of my life. Swedes are quite proud of being different in this way. Indeed, to a Swede, a government-enforced lock-down would probably have worked a great deal worse than the official (advisory) approach chosen.
So, businesses were told to have their employees work from home, and those that can do so have been implementing this. The recommendation remains in force until the end of the year, notably to reduce problems with public transport. Of direct effect on me, universities all immediately instituted online classes (instead of face-to-face), and this remains in force — Uppsala University is a pretty quiet place, these days. In a similar manner, senior high schools have had their students working from home (they are on summer holidays now, of course) — secondary schools are at risk of being important sources of infection (see
Contact tracing during coronavirus disease outbreak, South Korea, 2020).
On the other hand, of greatest surprise to me, it was decided to keep the junior (primary) schools operating normally. This has turned out very well, because there have been no reports of any students bringing Covid-19 home to their families. It is now accepted that young children are not usually infectious, contrary to the common belief at the beginning of the pandemic (
Children are not COVID-19 super spreaders: time to go back to school). This is one thing that Sweden apparently got right, contrary to actions in most other places in the world — disrupting the lives of young people is not a good thing.
In other quarantine actions, many places will now deliver your shopping order to your car, so you don't have to enter shops; and all open locations have signs about social distancing, and 1.5-meter (5 foot) marks on the floor. All public-access places have perspex screens between the service-provider and customer, and between customers; hand-washes are freely available; and cleaning services are now more strict and frequent. Most eating places serve customers outdoors only. We have been advised not to meet in groups, except outdoors, and even then there should be fewer than 50 people. All professional sporting activities have been postponed, along with other group activities, such as garden viewings (eg.
Öppen Trädgård 2020 inställt).
My local supermarket now opens one hour earlier on week-days, specifically for people in high-risk groups (such as myself) during that extra time. The accompanying sign is typically Swedish, in that it points out the purpose of opening early, and asks for co-operation from other customers, but also says that this will not be formally policed. As expected from Swedes, when my wife and I go there, almost all of the people are elderly, indicating that the others are, indeed, co-operating (or perhaps do not want to get up early).
Be realistic, would this type of voluntary approach actually work in your country? The only report of a major breach of quarantine was a party held to celebrate graduating from high school. The government recommended that these parties be avoided this year, much to the disappointment of the students, as this is always a big event. One group of c. 200 people ignored this advice, and thereby spread the virus among more than 40 people (
Coronasmitta spreds på stor studentfest). All countries have idiots.
There are practical problems to all of this, of course, just like in those places with full lock-downs. A personal one for me was the loss of my non-pension income. I used to help a Swedish academic with his English, but we have not met since the arrival of the virus in Sweden. I doubt that these meetings will ever resume, post-Covid.
Also, all travel has been restricted, which resulted in the cancellation of our long-planned trip to northern Sweden and Norway. All countries in Europe officially closed their borders for a few months. Within Sweden, typically, given what I have said above, we were not actually prevented from traveling, but were instead told that if we get sick we will have to be medically treated within our home county, which dissuaded everyone from going very far.
This has all changed in the past week. The ferries to Germany are now open; and it is summer holidays. This seems to have encouraged Swedes to come out of quarantine, and get on the move. This past weekend, it has become clear that relatives are visiting each other again (they are out cycling in family groups on my country roads, for example); and I have seen more caravans and campervans on the highways than I have at any time since last summer. Apparently, the summer destinations have started filling up with tourists, so this will be the test of how far Sweden has come (
Tusentals turister trängs på Gotlands gator).
As a final discussion point, I will mention that I actually live just outside of town, in a small community in the countryside. So, social distancing is not a practical problem for me, unless I go into town. In my local area, there have been 24 confirmed cases out of 3,007 people, which is an infection rate of 0.8%, which is the same rate as for Sweden as a whole.
However, this introduces the issue of the non-randomness of cases, which are quite definitely clustered (
A fraction of European regions account for a majority of covid deaths). Within Sweden, for example, Stockholm, as by far the largest city, has the highest death rate, as I will discuss below. So, the risks associated with infection depend very much on where you live. Sweden may have a small population, but its area is quite large, and spatial diversity is a real factor, just as it is in larger countries.
It is therefore a pity that all decisions within the European Union regarding the pandemic are done at the national level. A pandemic requires communal action, because any individual action can threaten the safety of the group as a whole. It has apparently one of the biggest "riddles" that the Buddhist countries of South-East Asia (Cambodia, Laos, Myanmar, Thailand, Vietnam) have been almost completely untouched by the pandemic that has spread to every other part of the globe (
Why has the pandemic spared the Buddhist parts of South-East Asia?); but anyone who has ever watched the co-operative way in which these communities function will not be surprised in the slightest.
It has therefore been the biggest disappointment that the European Union has been surprisingly non-united in its responses. At the moment, some countries are now open to visitors from some other countries, while residents of yet other countries are currently banned. None of this seems to be based on the actual case-rate data, but is much more to do with politics and how much money might be made during the summer holiday season. Greece, for example, is open to the British but not to Swedes, while Croatia is open to both. Needless to say, Croatia (and neighboring Montenegro) have had massive surges in cases in the past few weeks, since they are open to most holiday-makers, having had relatively few cases before — it is now no safer to be there than in much of Sweden.
[Aside: My wife and I came back from a holiday in Croatia on the same day that the main influx of the virus arrived in Sweden from northern Italy, where is was acquired by Swedes who had taken the school break week to go downhill skiing. The other large source in Scandinavia was via those people who had gone to Austria for the same purpose.]
Protecting the elderlyThis brings us to the biggest point of criticism within Sweden itself. This pandemic has highlighted very strongly just how badly elderly people are treated in this country. Put simply, I would never live in an aged-care home here, even if they were paying me, rather than the other way around.
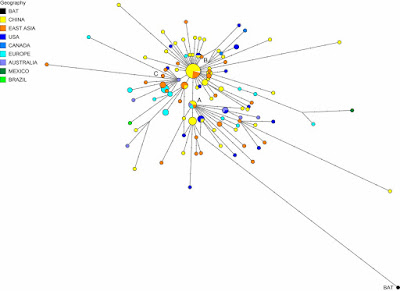
First, let's look at the current data on age-related Covid cases in Sweden (compiled by
Han Yin Lap). As you can see, 7.3% of the Covid-19 cases in Sweden have resulted in death, but 89.1% of those deaths have been in the 70+ age group. This is pretty much the same as elsewhere, sadly enough.
The problem in Sweden has been that the virus got into many of the aged-care homes long before anything was officially done about it. The government did not institute mandatory virus-testing of the staff (or even recommend it); and, as we now all know, it is the asymptomatic people who are the most dangerous in terms of spread. Furthermore, all reports (anecdotal as well as official) indicate that staff operational procedures were not modified before the middle of May, to protect either the patients or the staff (being a health-care worker is always risky:
How many healthcare workers have gotten coronavirus?).
You can imagine the outcome for yourself. The worst case was in Jönköping County. This is not a densely populated place by any means, but the case rate has been 1.2% of the people, compared to the national rate of 0.8%. The virus got into a large aged-care facility, of course. The highest death rates have been been in Stockholm County (0.10%) and Södermanland County (0.08%), compared to the national 0.05%, for exactly the same reason.
Closer to home, my local newspaper recently reported the data shown in the following table (Stora skillnad i hur hårt äldreboenden drabbats.
Upsala Nya Tidning, Lördag 4 juli 2020, p.6). Across 979 people in 20 aged-care facilities in Uppsala County, the death rate has been 5.8%, but varied from 0% to 18%. Only two facilities have so far reported no coronavirus-related deaths.
You can see why this has been a big discussion point, as this situation is by no means unusual in the other counties, except for Västerbotten (
Inte enbart en slump att Västerbotten har få döda i covid-19). Indeed, it is a national disgrace.
The issue here has been the lack of government-instituted testing. Sweden has a nationalized health-care system, and it does not work any better than such systems ever do. I once lay in a hospital ward for a day and a half, fully scrubbed and prepared for surgery, to have my appendix removed. When they finally got around to me, the knot on my surgery gown was so tight that they had to cut the cord to get the thing off (with a laugh, of course). I have other anecdotes of similar nature.
So, as far as the pandemic has been concerned, the national government dithered for months before deciding that they would, indeed, bear much of the financial cost of testing. Until then, only people with symptoms were tested for the virus. What is the point of that?!! We needed to know who had the virus and did not themselves know it, not those whom we were already sure had it.
Anyway, without national funding, the counties, who do the actual sampling, typically do nothing. This is how a national health scheme works (or does not). Fortunately, the government finally started testing more widely for the virus, which created a spike in reported cases in June, as noted in the first graph above.
Recently, the government agreed to fund testing for antibodies, for anyone who wants it. Only two counties, Uppsala and Stockholm, immediately implemented this idea, at the beginning of this month. Sadly, my wife and I have now been waiting for 3 weeks for the results of our tests. We were told: "it make take a week", which in the Swedish health-care system translates as: "don't hold you breath". We have, of course, been sent our bills, for our (smallish) part of the cost.
ConclusionSo, there you have it. Sweden has done no worse than a lot of other places, in spite of doing things somewhat differently. There was no government-enforced lock-down, but instead a government-advised voluntary quarantine. This has worked okay, and certainly much better than the government lock-down in the USA; but plenty of countries in Europe have had lower case rates. The death rate is a bit embarrassing, because old people are not treated well in Sweden. In that sense, what I am doing living in Sweden in my sixties? As Pete Townsend once noted (
My Generation): "I hope I die before I get old."
Note: For a slightly later but similar commentary by another local, see:
Sweden did not take herd immunity approach against coronavirus pandemic.